Navigating Healthcare Together: For Autistic Individuals and Providers
Key Points
- Autistic individuals face significant stress and sensory challenges in healthcare settings.
- Barriers include anxiety, communication difficulties, and sensory overload, leading to worse health outcomes.
- Healthcare providers can improve care with autism training, sensory-friendly environments, and clear communication.
- Use dim lighting, reduce noise, and create quiet areas to minimise sensory overload.
- Assume competence, use clear and literal language, and provide alternative communication methods.
- Autistic individuals can prepare for healthcare visits with questions, support persons and health profiles
Introduction
This article highlights the importance of self-advocacy and offers tips to help autistic individuals feel confident in navigating the healthcare system. It also details how healthcare staff can make the experience more inclusive for everyone. Simple changes can make a significant difference, as healthcare providers may encounter autistic patients at any time. This includes not only children but also autistic adults. Being prepared with the right information and approach is essential to providing the best care for autistic patients.

Understanding Autism in the Healthcare Context
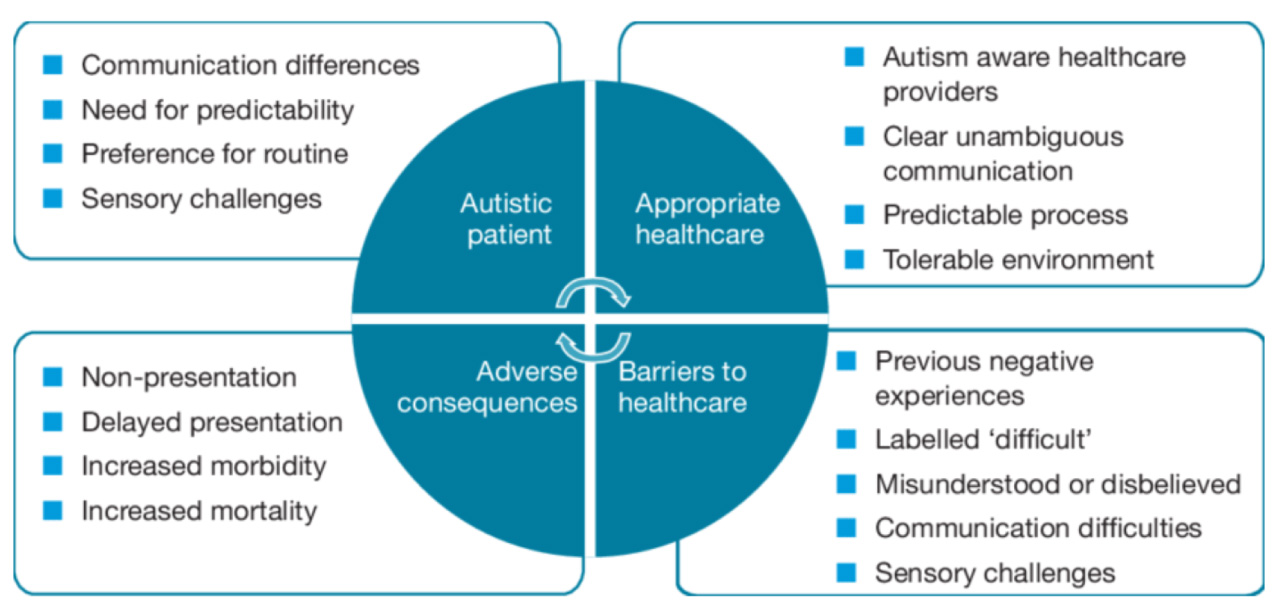
Image Credit: Understanding healthcare difficulties for autistic people: obstacles, impacts, and ways to improve care. (Extracted from Haydon et al, 2021)
Communication can be particularly challenging, as autistic individuals may struggle with understanding body language, vocal tones, and facial expressions, and may find eye contact uncomfortable. This can make it seem as though they are not listening or responding appropriately.
Therefore, it is crucial for healthcare providers to convey their messages in ways that are easily understandable for each autistic patient. Adapting to each patient’s needs is essential to optimise outcomes for both the healthcare provider and the patient.
Autism and Self-Advocacy in Healthcare
Healthcare providers need to understand autism better and use neurodiversity-affirming practices. However, it’s also important for autistic individuals to learn self-advocacy skills. Speaking up for yourself can be tough, but it helps ensure your needs are met and improves communication with healthcare providers.
These include things like:
- Write down your questions and concerns for the doctor.
- Bring a support person (family member, trusted friend/neighbour, caregiver) who understands your situation and can help with communication.
- Create a personal health profile (see example here) or use info cards (see example here) to organise and communicate your health information and needs. (See toolkits section for more resources.)
- Your doctor will need a full description of your symptoms to understand their cause and how to treat them. They typically ask for specific information about your symptoms.
- Use a worksheet like this one to think about your symptoms beforehand.
▫ Print and fill out a body map to indicate areas of pain or other sensations. - Make a checklist of things you will need to bring including your identification card, your medications (if any) and any items that will help make you more comfortable such as noise-cancelling headphones and your phone.
See Interoception and Self-Awareness in Autism to understand about using a body map to understand how your body feels.
During the Visit
- Walk through the clinic/hospital to become familiar with the layout and amenities.
- Ask to wait in the car or in a quiet room where you can control light and sound.
- Show the doctor your personal health profile or info cards if you have prepared one.
- Request explanations of policies and procedures, along with their reasons, to reduce anxiety and confusion.
- Ask for information to be repeated as needed for clarity and understanding and request it in written or emailed form for future reference.
Conclusion
References
- Arnold SR, Bruce G, Weise J, Mills CJ, Trollor JN, & Coxon K (2024). Barriers to healthcare for Australian autistic adults. Autism, 28(2), 301-315. https://doi.org/10.1177/13623613231168444
- McLean KJ, Haas M, Koenig J, Horvath M, Vigil M, Werner NE, & Bishop L (2024). “I’m dealing with a health care system that doesn’t get it”: Barriers and facilitators to inclusive healthcare for autistic adults. Autism, 28(6), 1382-1393.https://doi.org/10.1177/13623613241236380
- Haydon C, Doherty M & Davidson I. (2021). Autism: making reasonable adjustments in healthcare. British Journal of Hospital Medicine. 82. 1-11. 10.12968/hmed.2021.0314.
- Doherty M, Neilson S, O’Sullivan J, et al. (2022) Barriers to healthcare and self-reported adverse outcomes for autistic adults: a cross-sectional study. BMJ Open, 12(2):e056904. Published 2022 Feb 22. doi:10.1136/bmjopen-2021-056904
- Shaw SC, Carravallah L, Johnson M, et al. (2023). Barriers to healthcare and a ‘triple empathy problem’ may lead to adverse outcomes for autistic adults: A qualitative study. Autism, 28(7), 1746-1757.https://doi.org/10.1177/13623613231205629
Resources
Toolkits
- AASPIRE Healthcare Toolkit: Patient-Centred Care Tools for Autistic Adults. Academic-Autistic Spectrum Partnership in Research and Education (AASPIRE)
The Autism Healthcare Accommodations Tool (AHAT) generates customised reports for individuals with autism to give to their healthcare providers. It offers recommendations to improve healthcare experiences before, during, and after visits, based on a survey of each person’s needs. While designed for an American audience, many tips are also useful in a Malaysian setting. - National Autistic Society. My Health Passport
‘My Health Passport’ is a resource to help autistic people communicate their needs to healthcare professionals during hospital treatment. - Spectrum Intersections. Self-Advocacy in Healthcare: Personal Info cards
Personal Info cards help autistic individuals explain their needs to doctors, dentists, and other health professionals. They make it easier to communicate about health and treatment. The cards are grouped by common topics and allow users to choose what information to share. - Spectrum Intersections. Self-Advocacy in Healthcare: A toolkit for LGBTIQA+ autistic people, their family, carers, friends, support workers, and advocates
This toolkit, created by and for autistic LGBTIQA+ people, helps them navigate healthcare and self-advocate. It bridges gaps between them and healthcare professionals, ensuring informed consent within a patient-centred model.
Other Information
- Adult Autism Health Resources. Clinical Care for Autistic Adults: ASD Office Prep Tip Sheet. Harvard Medical School.
- All Brains Belong VT. Neuroinclusive Healthcare & Community
- Anita Lesko. Hospitals + Providers: How to Effectively Communicate With and Treat Autistic Patients. IBCCES
- Doherty M, McCowan S, Shaw SC. (2023) Autistic SPACE: a novel framework for meeting the needs of autistic people in healthcare settings. Br J Hosp Med (Lond). 84(4):1-9. doi:10.12968/hmed.2023.0006
Healthcare Experiences on the Spectrum
- Alisa Opar. How autistic adults are being let down by the healthcare system. Spectrum News.

